Overview

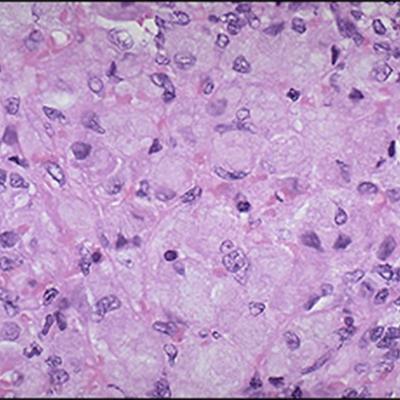
Lysosomes are compartments inside cells that act like waste disposal and recycling centers, breaking down cellular waste into components that can be reused or discarded. People with lysosomal storage disorders lack one or more key lysosomal enzymes. As a result, certain waste products accumulate in cells, leading to a variety of symptoms. In Gaucher disease, the deficient enzyme is glucocerebrosidase, which degrades the fatty molecule glucocerebroside (also known as glucosylceramide), a component of white and red blood cell membranes. Type 1 Gaucher disease primarily affects white blood cells called macrophages, which devour other worn-out cells. Macrophages filled with glucocerebroside collect in the liver and spleen, causing these organs to become enlarged and impairing their function. Symptoms range from mild to severe, appear anytime from childhood to adulthood, and also include severe anemia, easy bruising caused by low blood platelet count, and painful skeletal deformities. Two other forms of Gaucher disease affect cells in the brain as well, leading to neurological symptoms. These neuronopathic forms include Type 2 Gaucher disease, a severe disorder with onset in infancy or before birth, and Type 3 Gaucher disease, a milder form with later childhood or adult onset.
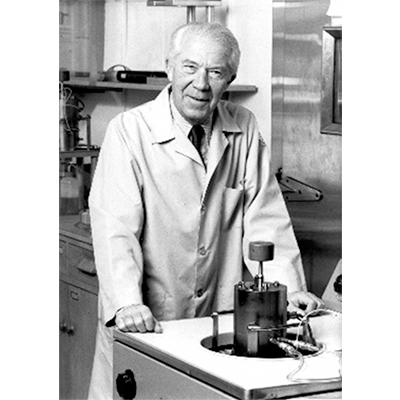
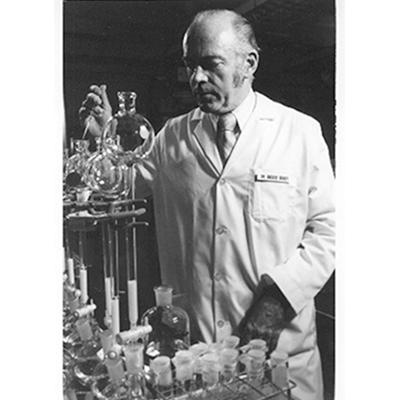
Physician-scientist Roscoe O. Brady (1923-2016) was an intramural investigator at NINDS who dedicated much of his career to understanding and developing treatments for lysosomal storage disorders. His work to identify the missing enzyme in Gaucher disease and determine how to replace the enzyme in cells that need it ultimately led to the development of alglucerase injection (Ceredase®, Genzyme) for the treatment of Type 1 Gaucher disease, the first enzyme replacement therapy (ERT) approved in the U.S. This accomplishment by Brady and his colleagues is all the more remarkable for how much persistence it required. Over twenty years passed from the discovery of the enzyme deficiency in Gaucher disease to the approval of Ceredase®, including eight years to purify enough enzyme for the first human tests and sixteen more years to obtain enough macrophage-targeted enzyme for the clinical trials that supported FDA approval. Brady’s career at NINDS exemplifies the ingenuity and long-term commitment necessary to develop promising approaches into safe and effective treatments.
Timeline
In his medical dissertation, French physician Philippe Gaucher first describes what will later become known as Gaucher disease1.

French chemist Henriette Aghion discovers that accumulation of a fatty substance called glucocerebroside causes enlarged spleens and livers in patients with Gaucher disease2.
Based on growing understanding of lysosomal enzyme uptake into different cell types, the enzyme is modified for improved targeting to macrophages19.
The FDA approves the orphan drug alglucerase (Ceredase®), an enzyme derived from human placenta, to treat Type 1 Gaucher disease22.

The FDA approves imiglucerase (Cerezyme®), a form of the enzyme produced using recombinant DNA technology25.
History of Development
Physician-scientist Roscoe O. Brady (1923-2016) was an intramural investigator at NINDS whose decades-long research on lysosomal storage disorders led to the first enzyme replacement therapy (ERT) for Type 1 Gaucher disease.
Tracking down a missing enzyme
Gaucher disease was first described in 1882, by budding French physician Phillipe Gaucher in his medical dissertation1. Over fifty years later in 1934, French chemist Henriette Aghion determined that a fatty molecule called glucocerebroside was the substance building up inside cells and causing enlarged spleens and livers in patients2. While this was a critical advance, the reason for the buildup remained unknown.
By the mid-1950s, physician-scientist Roscoe Brady had turned his attention to Gaucher disease in his laboratory at NINDS. After ruling out other explanations, he hypothesized that a defect in breaking down glucocerebroside was responsible for the disease. He teamed up with chemist David Shapiro from the Weizmann Institute in Israel to make glucocerebroside labeled with radioactive carbon, which they used to trace the molecule’s fate in cells from Gaucher patients and healthy controls. Through these experiments, Brady and his colleagues identified the enzyme glucocerebrosidase that cleaves glucocerebroside3 and showed that Gaucher disease results from deficient glucocerebrosidase activity4, 5, a finding independently confirmed by scientists in the UK6. This discovery had early implications for patients, as Brady and his colleagues soon developed a diagnostic test for Type I Gaucher disease7, as well as a prenatal test for Type 2 Gaucher disease8.
Knowing the cause of Gaucher disease also prompted Brady to suggest treatment through enzyme replacement therapy (ERT)9, an idea proposed as a general concept just two years earlier by Belgian scientist Christian deDuve10, who would later win the Nobel Prize in Physiology or Medicine for his discovery of the lysosome and efforts to characterize lysosomal enzymes11. In 1968, a study by Brady’s team and an extramural colleague determined that glucocerebrosidase is a lysosomal enzyme12, placing Gaucher disease among other conditions just being recognized as lysosomal storage disorders at the time.
Pioneering enzyme replacement therapy
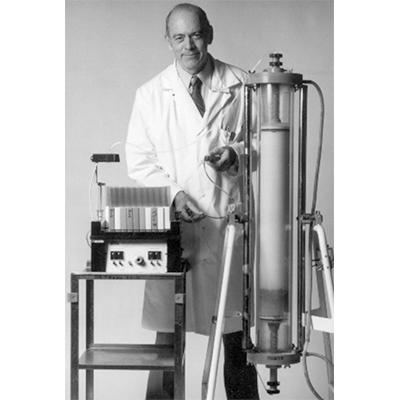
As a first step toward ERT for Gaucher disease, Brady’s team worked to isolate and purify glucocerebrosidase for initial tests in patients, and with support from the National Lipid Diseases Foundation (NLDF), they eventually developed a method to obtain small amounts of the enzyme from human placenta13. They delivered the enzyme intravenously to two patients with Gaucher disease and reported in 1974, that as hoped, the intervention reduced glucocerebroside accumulation in the patients’ livers14. These results represented important proof of principle for ERT, but Brady and his colleagues knew they would need much more enzyme for further tests than they could obtain using their current method.
After several more years, Brady’s team devised a new protocol to purify the enzyme from placenta in larger quantities15, but to their disappointment, tests of the enzyme in patients produced inconsistent results16. In Gaucher disease, glucocerebroside accumulates in cells called macrophages, a type of white blood cell. But back in the lab, Brady’s team and colleagues at the National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) found that the enzyme they were testing was not getting into these cells as efficiently as needed17. Based on growing understanding of the structure and transport of lysosomal enzymes18, they developed a way to modify certain molecular tags on glucocerebrosidase to improve its uptake into macrophages19.
In 1990, Brady and his team reported improvement across multiple clinical measures in a single child treated with the modified enzyme20. Concomitantly, the young biotechnology company Genzyme (now part of Genzyme Sanofi) had entered the scene. They worked to adapt Brady’s purification and modification procedures for commercial production of the enzyme and collaborated with NIH to conduct a subsequent trial in twelve individuals with moderate to severe Type 1 Gaucher disease. All participants in the trial showed dramatic improvement21, and in 1991, the FDA approved alglucerase (Ceredase®), an enzyme derived from human placenta, to treat Type 1 Gaucher disease22. The approval marked the first successful ERT for a lysosomal storage disorder.
Biotechnology and genetics research drive further advances
The development of Ceredase® was a remarkable feat, but Genzyme already understood that supply of the enzyme from human placenta would eventually be inadequate. Indeed, 20,000 placentas were required to purify enough enzyme to treat just one patient for one year. By this time, recombinant DNA technology had made it possible to obtain biological products through cell culture expression systems with higher efficiency than purification from tissue sources. In 1985, NINDS intramural investigator Edward Ginns and colleagues23, and separately, researchers funded by the National Cancer Institute (NCI)24, cloned and sequenced the human gene for glucocerebrosidase (GBA), paving the way for Genzyme to develop a recombinant form. The recombinant product Cerezyme®, was approved by the FDA25 in 1994, and shown to be as effective for the treatment of Type 1 Gaucher disease as placenta-derived Ceredase® . Today, Ceredase® is no longer produced26, but two additional forms of recombinant glucocerebrosidase have expanded treatment options for Type 1 Gaucher disease: velaglucerase alfa (VPRIV®, Shire) approved in 2010, and taliglucerase alfa (Elelyso®, Pfizer) approved in 2012.
Brady’s work with Gaucher disease served as a model for studying other lysosomal storage disorders. Brady helped identify the genetic causes of Niemann-Pick, Tay-Sachs, and Fabry diseases, and aided the development of ERTs for these previously untreatable disorders as well. Brady’s efforts also had lasting impact by spurring the early growth of the U.S. biotechnology industry. In recognition of his outstanding contributions, President George W. Bush awarded Brady the 2007 National Medal of Technology and Innovation, the nation’s highest honor for technological achievement27, 28.
Current research on Gaucher disease and other lysosomal storage disorders is building on the foundations laid by Brady, his NIH colleagues, and others. Although ERT is effective for Type 1 Gaucher disease, it does not address neurologic features of Types 2 and 3 Gaucher disease because current glucocerebrosidase formulations do not cross the blood brain barrier and are not readily taken up by neurons, even if delivered directly to the brain. Researchers therefore hope to develop new ways to target the therapy to the brain and other less accessible tissues. Investigators are also pursuing gene therapies for Gaucher disease and other lysosomal storage disorders, which if successful, would allow patients to produce missing enzymes on their own, without the need for chronic enzyme replacement. Additional efforts focus on small molecule drugs to improve the function of mutant glucocerebrosidase and on therapies to limit the production of glucocerebroside, the latter of which are already available for type 1 Gaucher disease.
Additional Information
Passing of a Great NINDS Physician-Scientist
NIH Office History website exhibit on Dr. Brady and Gaucher disease
List of References
Gaucher, PCE (1882) De l'epithelioma primitif de la rate, hypertrophie idiopathique del la rate san leucemie. MD thesis (Paris, France).
Aghion, Henriette (1934) La Maladie de Gaucher dans l'enfance (forme cardio-rénale). MD thesis (Paris, France).
Brady RO, Kanfer J, Shapiro D. The Metabolism of Glucocerebrosides. I. Purification and Properties of a Glucocerebroside-Cleaving Enzyme from Spleen Tissue. J Biol Chem. 1965 Jan; 240:39-43. PMID: 14253443 (NINDS intramural)
Brady RO, Kanfer J, Shapiro D. Metabolism of Glucocerebrosides. II. Evidence of an Enzymatic Deficiency in Gaucher’s Disease. Biochem Biophys Res Commun. 1965 Jan 18;18:221-5. PMID: 14282020 (NINDS intramural)
Brady RO, Kanfer JN, Bradley RM, Shapiro D. Demonstration of a deficiency of glucocerebroside-cleaving enzyme in Gaucher's disease. J Clin Invest. 1966 Jul;45(7):1112-5. PMID: 5338605 (NINDS intramural)
Show More
Short Communications. Biochem J. 1965 Nov;97(2):17C-24C. PMID: 16749131 (Non-U.S. support)
Kampine JP, Brady RO, Kanfer JN, Feld M, Shapiro D. Diagnosis of Gaucher's disease and niemann-pick disease with small samples of venous blood. Science. 1967 Jan 6;155(3758):86-8. PMID: 6015567 (NINDS intramural)
Schneider EL, Ellis WG, Brady RO, McCulloch JR, Epstein CJ. Infantile (type II) Gaucher's disease: in utero diagnosis and fetal pathology. J Pediatr. 1972 Dec;81(6):1134-9. PMID: 4674572 (NINDS intramural; NIH/NINDS, grant NS05227; NICHD career development award; John A. Hartford Foundation; March of Dimes; University of California Cancer Research Fund; Maternal and Child Service, United States Public Health Service)
Brady RO. The sphingolipidoses. N Engl J Med. 1966 Aug 11;275(6):312-8. PMID: 5940695 (NINDS intramural)
DeDuve C. From Cytases to Lysosomes. Fed Proc. 1964 Sep-Oct; 23:1045-9. PMID: 14209796
Physiology or Medicine 1974 - Press Release. Nobelprize.org. Available at https://www.nobelprize.org/nobel_prizes/medicine/laureates/1974/press.html (Accessed 23 February 20)
Weinreb NJ, Brady RO, Tappel AL. The lysosomal localization of sphingolipid hydrolases. Biochim Biophys Acta. 1968 Apr 24;159(1):141-6. PMID: 5650428 (NINDS intramural; NIH/NIAMS, grant AM05609)
Pentchev PG, Brady RO, Hibbert SR, Gal AE, Shapiro D. Isolation and characterization of glucocerebrosidase from human placental tissue. J Biol Chem. 1973 Aug 10;248(15):5256-61. PMID: 4768898 (NINDS intramural, National Lipid Diseases Foundation)
Brady RO, Pentchev PG, Gal AE, Hibbert SR, Dekaban AS. Replacement therapy for inherited enzyme deficiency. Use of purified glucocerebrosidase in Gaucher's disease. N Engl J Med. 1974 Nov 7;291(19):989-93. PMID: 4415565 (NINDS intramural, National Lipid Diseases Foundation)
Furbish FS, Blair HE, Shiloach J, Pentchev PG, Brady RO. Enzyme replacement therapy in Gaucher's disease: large-scale purification of glucocerebrosidase suitable for human administration. Proc Natl Acad Sci U S A. 1977 Aug;74(8):3560-3. PMID: 269414 (NINDS intramural, National Lipid Diseases Foundation)
Brady RO. Enzyme replacement in the sphingolipidoses. In: Barranger JA, Brady RO, eds. The molecular basis of lysosomal storage disorders. Orlando, Fla.: Academic Press, 1984:461–78.
Furbish FS, Steer CJ, Barranger JA, Jones EA, Brady RO. The uptake of native and desialylated glucocerebrosidase by rat hepatocytes and Kupffer cells. Biochem Biophys Res Commun. 1978 Apr 14;81(3):1047-53. PMID: 666784 (NIH/NINDS/NIAMS, intramural)
Stahl PD, Rodman JS, Miller MJ, Schlesinger PH. Evidence for receptor-mediated binding of glycoproteins, glycoconjugates, and lysosomal glycosidases by alveolar macrophages. Proc Natl Acad Sci U S A. 1978 Mar;75(3):1399-403. PMID: 274729 (NIH/NCI/NIGMS/NHLBI, grants CA12858, GM21096, HL56343)
Furbish FS, Steer CJ, Krett NL, Barranger JA. Uptake and distribution of placental glucocerebrosidase in rat hepatic cells and effects of sequential deglycosylation. Biochim Biophys Acta. 1981 Apr 3;673(4):425-34. PMID: 6784774. (NIH/NINDS/NIAMS, intramural)
Barton NW, Furbish FS, Murray GJ, Garfield M, Brady RO. Therapeutic response to intravenous infusions of glucocerebrosidase in a patient with Gaucher disease. Proc Natl Acad Sci U S A. 1990 Mar;87(5):1913-6. PMID: 2308952 (NINDS intramural)
Barton NW, Brady RO, Dambrosia JM, Di Bisceglie AM, Doppelt SH, Hill SC, Mankin HJ, Murray GJ, Parker RI, Argoff CE, et al. Replacement therapy for inherited enzyme deficiency--macrophage-targeted glucocerebrosidase for Gaucher's disease. N Engl J Med. 1991 May 23;324(21):1464-70. PMID: 2023606 (NIH/NINDS/NIDDK/CC, intramural; National Gaucher Foundation; Genzyme)
U.S. Food and Drug Administration. Drugs@FDA: FDA Approved Drug Products. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=020057 (Accessed 23 February 2018)
Tsuji S, Choudary PV, Martin BM, Winfield S, Barranger JA, Ginns EI. Nucleotide sequence of cDNA containing the complete coding sequence for human lysosomal glucocerebrosidase. J Biol Chem. 1986 Jan 5;261(1):50-3. PMID: 3001061 (NINDS intramural)
Sorge J, West C, Westwood B, Beutler E. Molecular cloning and nucleotide sequence of human glucocerebrosidase cDNA. Proc Natl Acad Sci U S A. 1985 Nov;82(21):7289-93. PMID: 3864160 (NIH/NCI, grant CA3644; March of Dimes Birth Defects Foundation)
U.S. Food and Drug Administration. Drugs@FDA: FDA Approved Drug Products. Available at: https://www.accessdata.fda.gov/scripts/cder/daf/index.cfm?event=overview.process&ApplNo=020367 (Accessed 23 February 2018)
Grabowski GA, Barton NW, Pastores G, Dambrosia JM, Banerjee TK, McKee MA, Parker C, Schiffmann R, Hill SC, Brady RO. Enzyme therapy in type 1 Gaucher disease: comparative efficacy of mannose-terminated glucocerebrosidase from natural and recombinant sources. Ann Intern Med. 1995 Jan 1;122(1):33-9. PMID: 7985893 (NINDS intramural; NIH/NCRR, grant RR000071)
Samulski, C. Roscoe Brady. National Science and Technology Medals Foundation. Available at https://www.nationalmedals.org/laureates/roscoe-brady# (Accessed 23 February 2018)
Garnett, Shannon E. (2008). Brady Receives Presidential Honor for Scientific Achievement. NIH Record (Vol. LX, No. 22), 31 October [online]. Available at https://nihrecord.nih.gov/newsletters/2008/10_31_2008/story5.htm (Accessed 23 February 2018)