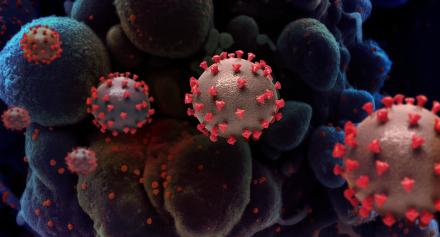
In 2019, a new coronavirus called ‘SARS-CoV-2’ quickly spread worldwide. Infection by this virus causes the disease known as COVID-19. COVID-19 primarily targets the respiratory system, but it also affects the nervous system and other organs. Most cases of COVID-19 are mild, especially in those who have been vaccinated, and go away within a couple of weeks. However, severe cases of COVID-19 can damage a person’s organs. When COVID-19 affects the lungs, it prevents the body from getting enough oxygen, which can lead to disability or death.
Some people have symptoms of COVID-19 that last for weeks, months, or even years after their initial infection. Some may develop new symptoms after an initial recovery or after mild initial COVID 19. These prolonged symptoms are known as “Long COVID,” which can affect many parts of the body, particularly the brain and nervous system. Medical and research communities are studying how COVID-19 might cause or contribute to the neurological symptoms of Long COVID. Researchers hope to better understand this connection to support diagnosis and develop effective treatments for people experiencing Long COVID.
Read below to understand what we know about COVID-19’s effects on the brain and nervous system, and promising avenues of study to understand and treat Long COVID.
What do we know about the effects of SARS-CoV-2 and COVID-19 on the nervous system?
COVID-19 can have a wide variety of effects on the nervous system. People who have severe enough COVID-19 to require hospitalization may have lung, kidney, or other organ damage that can also affect the brain (known as metabolic encephalopathy). This happens when the brain does not get enough oxygen, or problems in other organs change the balance of chemicals in the brain. People with severe COVID-19 may also develop strokes due to a tendency for increased clot formation, which can block the flow of blood and oxygen to the brain.
After the initial infection, during what’s known as the subacute phase, people who have had COVID-19 may develop a variety of inflammatory syndromes affecting the brain, spinal cord, or nerves.
- When the inflammation affects multiple areas within the brain it is called acute disseminated encephalomyelitis. When the damage is severe enough to cause bleeding in the brain, this is known as acute necrotic hemorrhagic encephalitis. In rare cases, the inflammation may affect only the thalamus, which sends and receives movement and sensory information.
- If the inflammation affects the spinal cord it can lead to a condition called transverse myelitis. If the inflammation only affects the motor nerves it can cause paralysis that travels from the outer limbs towards the trunk (ascending paralysis). This is called Guillain-Barré Syndrome.
In children, the inflammatory process can affect multiple organ systems and is called multi-inflammatory syndrome in children (MIS-C). It is important to recognize these syndromes early in the course of the illness since they can be treated with drugs that target inflammation.
Scientists are still learning how COVID-19 affects the nervous system. You can read the NINDS Director’s Message on Understanding neurological complications of COVID-19 to learn about research NINDS is supporting to better understand this connection.
Funding opportunities include new analyses of large brain COVID-19 datasets, how COVID-19 affects pre-existing neurological conditions, and how COVID-19 affects nervous systems and mood disorders in different stages of the disease.
Does COVID-19 affect the nervous system of certain populations differently?
COVID-19 had an outsized impact on populations designated by the NIH to experience health disparities. This includes racial and ethnic minority groups, socioeconomically disadvantaged populations, and people living with disabilities. These groups face more COVID-19 risks, like neurological complications, for many reasons. Existing or untreated health issues in these populations—including diabetes, heart disease, and prior stroke—put them at higher risk for adverse outcomes. Social determinants of health also contribute to higher rates of infection, serious complications, and death. Social determinants of health are things like limited access to healthcare, medical discrimination, unconscious bias in healthcare, and communal living. Learn more about NINDS Social Determinants of Health Framework for Addressing Health Inequities(pdf, 1363 KB). NINDS and other components of NIH are funding research to better understand what drives these health disparities in COVID-19. This includes research at a population level and learning more about risks we may not yet understand.
To learn more about how NIH defines health disparities, see the National Institute on Minority Health and Health Disparities (NIMHD) definitions page on this topic.
Am I at a higher risk if I currently have a neurological disorder?
COVID-19 is a new disease, so researchers are still studying the risks for people already living with a neurological disorder. According to the Centers for Disease Control and Prevention (CDC), people living with dementia or Alzheimer’s disease, or who have had a stroke, are at higher risk for severe COVID-19.
While some data suggest that people with existing neurological disorders are at higher risk of getting COVID-19 or experiencing worse symptoms, this connection is not fully understood. To learn more about what health conditions may put you at greater risk for severe COVID-19, see the CDC guidelines on people with certain medical conditions.
What are possible long-term neurological complications of COVID-19?
COVID-19 can affect many parts of the body. Researchers are learning more about the long-term effects of COVID-19 on the brain and nervous system and whether those who have experienced COVID 19 are at greater risk for other diseases. Those who experience severe COVID-19 or are hospitalized are more likely to have symptoms that last beyond their initial infection. However, those with mild cases may also develop new or worsening Long COVID symptoms.
How Long COVID changes over time varies from person to person. Some people improve within weeks, while others may still have symptoms for years after their initial infection. Sometimes Long COVID symptoms come back after they have gone away or get worse over time. Researchers may use the term “post-acute sequelae of SARS-CoV-2,” or PASC, in studies exploring the potential long-term consequences of COVID-19.
Long COVID is a “diagnosis of exclusion,” meaning it is diagnosed only after a doctor has ruled out other possible causes for symptoms. It is also possible that Long COVID or COVID-19 can help uncover diseases that a person did not know they had. While there is currently no standard treatment for Long COVID, the symptoms of Long COVID can be treated. Individuals with Long COVID should talk with their doctor about what treatments work best for managing their symptoms.
The most common neurological symptoms of Long COVID include:
Cognitive symptoms of Long COVID
Brain fog
People with COVID-19 may experience new or increased difficulty concentrating, processing information, and remembering things. This is sometimes called “brain fog” and can last for weeks or months after infection.
Sleep disturbances
Approximately 40% of people with Long COVID report major changes to their sleep after COVID-19 . Sleep is important for the brain, and sleep disorders can contribute to fatigue and cognitive difficulties.
Learn more about efforts by NINDS and the National Institute on Aging (NIA) to understand the relationship between sleep and Long COVID.
Anxiety, depression, and stress
People who have had COVID-19 may experience mood disorders for the first time. Researchers are investigating whether there is a connection between the effects of Long COVID on the brain and depression or anxiety. Click here to read more about mental health and COVID-19 and get NIH resources that can help.
Fatigue and Long COVID
Many diseases from viral infections, like COVID-19, can cause feelings of exhaustion or exercise intolerance. Both during a COVID-19 and with Long COVID, people may feel they have less of an energy reserve. This fatigue is often severe enough to interfere with a person’s daily life.
Post-exertional malaise
Some people who have recovered from COVID-19 describe feeling very tired or a worsening of symptoms after only a little bit of physical, cognitive, emotional, or social activity. This is called post-exertional malaise, or PEM, and is a common symptom of Long COVID.
Pain, Sensitivity, and Movement Symptoms of Long COVID
Sensitivity and Pain
People with Long COVID may experience new pain or loss of sensitivity to touch. They also may experience tingling or burning sensations. These changes tend to be worse in the limbs, particularly in the hands, and/or feet. This is because COVID-19 is thought to affect the nerves that send signals like touch, pressure, heat/cold, and pain to the brain.
Headache
Headaches can accompany COVID-19. Some people with Long COVID continue to have mild to severe headaches. These headaches may feel different from a migraine. The frequency of headaches varies by individual. In some individuals, the headaches may be related to blood clots that have formed in the vessels surrounding the brain (known as venous sinuses).
Dizziness/Fainting
For some people with Long COVID, the part of the nervous system that regulates involuntary things like heart rate and blood pressure may not function as well. This is called dysautonomia and can lead to increased heart rate and dizziness or fainting when standing up from a lying down or sitting position. This type of dizziness/fainting is called postural orthostatic tachycardia syndrome (POTS).
Trouble with Movement
Since COVID-19 can affect the nervous system, it can also affect how the brain sends signals to the muscles of the body to coordinate movement. Some people with Long COVID have trouble with coordination (ataxia), loss of movement (bradykinesia), tremor, or sudden muscle twitching or jerking (myoclonus).
How are Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) related?
Some of the symptoms of Long COVID and ME/CFS can be very similar. Fatigue, post-exertional malaise, sleep problems, and POTS may occur in Long COVID and in ME/CFS. As with Long COVID, many people report an onset of ME/CFS symptoms after an illness due to an infection. By understanding what changes in the body cause Long COVID, researchers hope to address unanswered questions for people living with ME/CFS and other poorly understood chronic post-infection illnesses. Read more about how NINDS is leading studies to try and understand this critical connection.
What research is NIH doing on Long COVID?
NINDS is funding cutting-edge research to explore potential connections between the effects of COVID-19 on blood vessels in the brain and similar effects on the lining of the intestines, and whether this damage may relate to chronic cognitive symptoms of Long COVID. Read the most recent finding from this study.
NINDS is also investing in new tools to understand the biological effects of COVID-19. This includes research to define the biological basis of Long COVID symptoms using MRI and blood biomarkers. The institute is also funding research to evaluate the neurological complications of COVID-19 using neuroimaging, neuropsychiatric examination, and cognitive testing. This research also aims to further explore how different characteristics such as sex, BMI, race/ethnicity, and socioeconomic status, play a role in neurocognitive changes.
NIH’s Researching COVID to Enhance Recovery (RECOVER)) Initiative is a national, patient-centered effort to understand the causes of Long COVID and advance discovery of treatments for Long COVID. NINDS is a leading partner in this effort. RECOVER seeks to identify treatments for all individuals affected by Long COVID, including those disproportionately affected by COVID-19. RECOVER is leading observational studies to track Long COVID symptoms and outcomes over time, as well as clinical trials to test potential treatments, and pathobiology studies to understand the biological causes of Long COVID. One example of a clinical trial is RECOVER-NEURO, which seeks to advance our understanding of how COVID-19 affects the brain and identify potential treatments for symptoms like brain fog. Learn how people with Long COVID, their family members, and healthy volunteers can participate in RECOVER.
NINDS and NIH are part of the US Department of Health and Human Services (HHS), which is coordinating a whole-of-government approach to respond to the longer-term impacts of COVID-19 through the Office of Long COVID Research and Practice. You can sign up for updates on this office and its work at their website.
What can I do to reduce my risk for COVID-19 and Long COVID?
Almost everyone should get vaccinated against COVID-19. COVID-19 vaccination continues to be the best way to protect against serious illness and may help prevent or lessen Long COVID symptoms. Most side effects of the vaccine are temporary and go away within a few days. The U.S. Food and Drug Administration (FDA) and CDC continue to investigate any report of adverse consequences of the vaccine through the Vaccine Adverse Event Reporting System, or VAERS. Talk with your doctor if you have any pre-existing known allergic or severe reactions to this or other vaccines.
See more information on Long COVID from the NIH and from the CDC.
