New deep brain stimulation device coupled with powerful AI may improve therapy for treatment-resistant depression
Using a novel deep brain stimulation (DBS) device capable of recording brain signals, researchers have identified a pattern of brain activity or “biomarker” related to clinical signs of recovery from treatment-resistant depression. The findings from this small study are an important step towards using brain data to understand a patient’s response to DBS treatment. The study was published in Nature and supported by the National Institutes of Health’s Brain Research Through Advancing Innovative Neurotechnologies® (BRAIN) Initiative, or The BRAIN Initiative®.
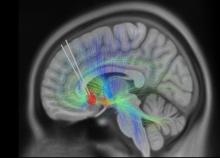
Although the approach is still experimental, clinical research shows that DBS can be used safely and effectively to treat cases of depression in which symptoms have not improved with antidepressant medications, referred to as treatment-resistant depression. People receiving DBS undergo surgery to have a thin metal electrode implanted into specific brain areas to deliver electrical impulses that modulate brain activity. How exactly DBS improves symptoms in people with depression is not well-understood, which has made it difficult for researchers to objectively track patients’ response to treatment and adjust as needed.
The small study enrolled 10 adults with treatment-resistant depression, all of whom underwent DBS therapy for six months. Each participant received the same stimulation dose to begin and then stimulation levels were increased once or twice. Later, researchers used artificial intelligence (AI) tools to analyze collected brain data from six patients and observed a common brain activity signature or biomarker that correlated with patients self-reporting feeling symptoms of depression or stable as they recovered. In one patient, researchers identified the biomarker and were retrospectively able to predict that a patient would fall back into a major depressive episode four weeks before clinical interviews showed they were at risk of a relapse occurring.
“This study demonstrates how new technology and a data-driven approach can refine DBS therapy for severe depression, which can be debilitating,” said John Ngai, Ph.D., director of the BRAIN Initiative. “It’s this type of collaborative work made possible by the BRAIN Initiative that moves promising therapies closer to clinical use.”
In the study, patients received DBS targeting the subcallosal cingulate cortex (SCC), a brain region that regulates emotional behavior and is involved in feelings of sadness. DBS of the SCC is an emerging therapy that can provide stable, long-term relief from depressive symptoms for years. However, using DBS to treat depression remains challenging because each patient’s path to stable recovery looks different. Clinicians also must rely on subjective self-reports from patient interviews and psychiatric rating scales to track symptoms, which can fluctuate over time. This makes it hard to distinguish between normal mood variations and more serious situations requiring a tweak in stimulation. In addition, changes in symptoms in response to DBS can take weeks or months to occur, making it difficult to tell how well the therapy is working.
“This biomarker suggests that brain signals can be used to help understand a patient’s response to DBS treatment and adjust the treatment accordingly,” said Joshua A. Gordon, M.D., Ph.D., director of NIH’s National Institute of Mental Health. “The findings mark a major advance in translating a therapy into practice.”
The patients in the study responded well to DBS therapy; after six months, 90% showed a significant improvement in depression symptoms, and 70% were in remission or no longer depressed. This high response rate was a unique opportunity to look back and examine how each patient’s brain responded differently to the stimulation during treatment.
Christopher Rozell, Ph.D., Julian T. Hightower Chair and professor of electrical and computer engineering at Georgia Tech in Atlanta, and his colleagues used a technique called explainable artificial intelligence to understand these subtle changes in brain activity. The algorithm used brain data to distinguish between depressive versus stable recovery states and was able to explain what activity changes in the brain were the main drivers of this transition. Importantly, the biomarker also distinguished between normal day-to-day transient mood changes and sustained worsening symptoms. This algorithm could provide clinicians with an early warning signal that a patient is moving toward a highly depressive state and requires a DBS adjustment and extra clinical care.
“Nine out of 10 patients in the study got better, providing a perfect opportunity to use a novel technology to track the trajectory of their recovery,” said Helen Mayberg, M.D., director of the Nash Family Center for Advanced Circuit Therapeutics at Icahn Mount Sinai in New York City and co-senior author of the study. “Our goal is to identify an objective, neurological signal to help clinicians decide when, or when not, to make a DBS adjustment.”
“We showed that by using a scalable procedure with single electrodes in the same brain region and informed clinical management, we can get people better,” said Dr. Rozell, co-senior author of the study. “This study also gives us an amazing scientific platform to understand the variation between patients, which is key to treating complex psychiatric disorders like treatment-resistant depression.”
Next, the team analyzed data from MRI brain scans collected from patients before surgery. The results revealed structural and functional abnormalities in the specific brain network targeted by the DBS therapy. More severe white matter deficits were related to longer recovery times.
Researchers also used AI tools to analyze changes in facial expression extracted from videos of participant interviews. In a clinical setting, a patient’s facial expression can reflect the severity of their depression symptoms, a change that psychiatrists likely pick up on in routine clinical evaluations. They found patterns in individual patient expressions that coincided with their transition from illness to stable recovery. This could serve as an additional tool and new behavioral marker to track recovery in DBS therapy. More research is needed to determine whether the video analysis can reliably predict current and future disease states.
Both the observed facial expression changes and anatomical deficits correlated with cognitive states captured by the biomarker, supporting the use of this biomarker in managing DBS therapy for depression.
The research team, including Drs. Mayberg and Rozell, and Patricio Riva-Posse, M.D., at Emory University School of Medicine in Atlanta, is now confirming their findings in a second cohort of patients at Mount Sinai. Future studies will continue to explore the antidepressant effects of DBS by using a next-generation device to study the neural basis of moment-to-moment changes in mood.
According to the research team, this study represents a significant advance in early-stage DBS therapy for various mental disorders, including severe depression, obsessive-compulsive disorder, post-traumatic stress disorder, binge eating disorder, and substance use disorder. Other DBS studies have identified brain biomarkers for chronic pain, but using brain data to successfully treat patients is still under development.
The study was supported by the NIH BRAIN Initiative (UH3NS103550), the National Science Foundation, the Hope for Depression Research Foundation, and the Julian T. Hightower Chair at Georgia Tech.
Article:
Alagapan, S, et al. Cingulate dynamics track depression recovery with deep brain stimulation. Nature, September 20, 2023. DOI: 10.1038/s41586-023-06541-3.
The NIH BRAIN Initiative is managed by 10 Institutes and Centers whose missions and current research portfolios complement the goals of The BRAIN Initiative®: National Center for Complementary and Integrative Health, National Eye Institute, National Institute on Aging, National Institute on Alcohol Abuse and Alcoholism, National Institute of Biomedical Imaging and Bioengineering, Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institute on Drug Abuse, National Institute on Deafness and other Communication Disorders, National Institute of Mental Health, and National Institute of Neurological Disorders and Stroke.
NINDS is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit the NIH website.
