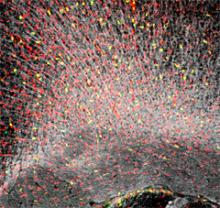
Scientists found that normal neuronal firing patterns can enhance the growth of brain tumors. Courtesy of Monje lab, Stanford University School of Medicine, CA
NIH-funded study opens new path to discovering brain cancer treatments
Using human brain tumor samples, scientists have discovered that normal patterns of nerve cell firing may enhance the growth of cancer cells. They also found that, neuroligin-3 (NLGN3), a gene known to be important for brain cell communication, may influence tumor growth and patient survival, making it a potential new target for therapy. The study, published in Cell, was partially funded by the National Institutes of Health (NIH).
“We found that tumors may hijack the brain’s regular firing patterns used daily for thinking, feeling and moving,” said Michelle Monje, M.D., Ph.D., assistant professor of neurology and neurological sciences at Stanford University School of Medicine, CA, and the senior author of the study. “It’s a striking example of an organ’s core function fueling the cancer arising within it.”
In this study, Dr. Monje’s team studied a variety of high-grade gliomas, the most lethal forms of brain cancer. They found that secretion of neuroligin-3, a protein known to physically connect nerve cells at communication points, or synapses, may be a critical step linking neuronal firing to the growth of many high-grade gliomas. Supporting evidence also suggested that patients whose tumors had low levels of the neuroligin-3 gene lived longer than those whose tumors had high levels.
“These types of gliomas are devastating and very few patients survive them,” said Jane Fountain, Ph.D., program director, National Institute of Neurological Disorders and Stroke (NINDS), part of the NIH, which supported the study. “Dr. Monje’s research is the first to show that neurons are important for glioma growth and provides a surprising new role for neuroligin-3.”
The scientists obtained a variety of high-grade glioma samples from 10 patients diagnosed between 2 and 70 years of age. They implanted cells from a tumor sample into the premotor cortex of animal models, and next to nerve cells genetically engineered to fire in response to flashes of laser light.
They found that they could make the cancer cells reproduce faster by stimulating the firing of neighboring nerve cells. Cancer cells located within the light-activated neural circuit grew more rapidly than the ones that were outside of the circuit or located in the brains of control animals. When they repeated the stimulation over seven days they found a greater mass of cancer cells in the active neural circuit.
Previously, Dr. Monje’s lab found that using light to stimulate similar neuronal firing patterns improved a mouse’s walking speed and triggered the birth of stem cells which develop into brain support cells called glia. These types of glia normally insulate nerves by wrapping around, or myelinating them. They also have the potential to develop into several forms of glioma.
“Our results suggested that the same firing patterns that can help a mouse learn to walk better also promote the growth of brain cancers. The tumor cells are co-opting these mechanisms of neural plasticity,” said Dr. Monje.
Dr. Monje’s team obtained similar results when they tested the effects of factors secreted by neurons firing in living samples of cortical slices. Each type of cancer cell tested grew faster when it was exposed to factors secreted in response to neuronal activity. The researchers also showed that they could slow cancer cell proliferation by blocking all nerve cells from firing when they treated the slices with a chemical called tetrodotoxin.
When the scientists searched the nutrient liquids in which the brain slices were kept alive, they found several factors that promote glioma growth were released as a result of neural activity. Of these, neuroligin-3 protein was the most potent and stimulated the proliferation of the largest number of the tumor samples. Conversely, blocking neuroligin-3 inhibited the proliferation induced by neuronal firing. Further experiments showed that treating some of the cancer cells with neuroligin-3 in turn caused them to make more of their own neuroligin-3.
“We were very surprised,” said Dr. Monje. “When we started the experiments we never thought that neuroligin-3 might influence tumor growth.”
Dr. Monje and her colleagues also analyzed information on 429 brain cancer cases stored in The Cancer Genome Atlas (TCGA), an advanced library of cancer genomic information hosted by the NIH’s National Cancer Institute (NCI) and National Human Genome Research Institute. They found that brain cancer patients whose tumors had made, or expressed, fewer messenger RNA copies of the neuroligin-3 gene lived longer than patients with more copies.
Mutations in the neuroligin-3 gene have been linked to autism. By searching additional cancer databases, the scientists also found evidence suggesting that the neuroligin-3 gene may be linked to other cancers including those of the thyroid, pancreas, prostate, and stomach.
Finally, the scientists showed that they could block brain tumor cell growth by treating the cells with drugs that inhibit cancer genes turned on by neuroligin-3.
“We showed that neuroligin-3 may be the fuel that stokes the growth of brain cancers,” said Dr. Monje. “Our results provide hope that we can one day impede tumor growth. We must find a way to target specific neuron-glioma interactions therapeutically.”
According to the NCI, in 2011 an estimated 144,463 people in the United States were living with brain or other nervous system cancers. Dr. Monje and her colleagues are seeking to develop neuroligin-3-based therapeutic strategies in ongoing preclinical work.
This work was supported by grants from the NINDS (NS070926), McKenna Claire Foundation, Matthew Larson Foundation, National Science Foundation, Godfrey Family Fund in Memory of Fiona Penelope, California Institute for Regenerative Medicine, Alex’s Lemonade Stand Foundation, The Cure Starts Now Foundation, Lyla Nsouli Foundation; the Dylan Jewett, Connor Johnson, Zoey Ganesh, Dylan Frick, Abigail Jensen, Wayland Villars, and Jennifer Kranz Memorial Funds, Unravel Pediatric Cancer, Virginia and D.K. Ludwig Fund for Cancer Research, the Bear Necessities Pediatric Cancer Foundation, Lucile Packard Foundation for Children’s Health, Child Health Research Institute at Stanford, Anne T. and Robert M. Bass Endowed Faculty Scholarship in Pediatric Cancer and Blood Diseases.
- by Christopher G. Thomas, Ph.D.
References:
Venkatesh et al. “Neuronal activity promotes glioma growth through neuroligin-3 secretion,” Cell, May 7, 2015. DOI:10.1016/j.cell.2015.04.012
For more information on brain cancer, visit Brain and Spinal Tumors Information Page.
###
The NINDS (http://www.ninds.nih.gov) is the nation’s leading funder of research on the brain and nervous system. The mission of NINDS is to seek fundamental knowledge about the brain and nervous system and to use that knowledge to reduce the burden of neurological disease.
About the National Institutes of Health (NIH): NIH, the nation's medical research agency, includes 27 Institutes and Centers and is a component of the U.S. Department of Health and Human Services. NIH is the primary federal agency conducting and supporting basic, clinical, and translational medical research, and is investigating the causes, treatments, and cures for both common and rare diseases. For more information about NIH and its programs, visit http://www.nih.gov.
