What is a traumatic brain injury (TBI)?
A traumatic brain injury (TBI) refers to a brain injury that is caused by an outside force. A forceful bump, blow, or jolt to the head or body can cause it, but not all blows or jolts to the head result in a TBI. An object entering the brain can also cause a TBI. TBIs are sometimes called brain injuries or even head injuries.
Some types of TBI can cause temporary or short-term problems with brain function, including problems with how a person thinks, understands, moves, communicates, and acts. More serious TBIs can lead to severe and permanent disability—and even death.
Some TBIs are considered primary, meaning the damage is immediate. Others can be secondary, meaning they can happen gradually over the course of hours, days, or weeks after injury. These secondary TBIs are the result of reactive processes that happen after the initial head trauma.
There are two broad types of TBIs:
- Penetrating TBI (also known as open TBI) happens when an object pierces the skull (such as a bullet, shrapnel, or bone fragment) and enters the brain tissue. Penetrating TBI typically damages only part of the brain.
- Non-penetrating TBI (also known as closed head injury or blunt TBI) is caused by an external force strong enough to move the brain within the skull. Causes include falls, motor vehicle crashes, sports injuries, blast injury, or being struck by an object.
Some accidents or trauma can cause both penetrating and non-penetrating TBI in the same person.
Signs and symptoms of TBI
Headache, dizziness, confusion, and fatigue tend to start immediately after an injury but resolve over time. Emotional symptoms such as frustration and irritability tend to develop during recovery.
Seek immediate medical attention if the person experiences any of the following symptoms, especially within the first 24 hours after an injury to the head:
Physical symptoms of TBI
- Headache
- Convulsions or seizures
- Blurred or double vision
- Unequal eye pupil size or dilation
- Clear fluids draining from the nose or ears
- Nausea and vomiting
- New neurological problems (such as slurred speech, weakness of arms, legs, or face, or loss of balance)
Cognitive and behavioral symptoms of TBI
- Loss of or change in consciousness for anywhere from a few seconds to a few hours
- Decreased level of consciousness (like being hard to wake up)
- Confusion or disorientation
- Problems remembering, concentrating, or making decisions
- Changes in sleep patterns (such as sleeping more, difficulty falling or staying asleep, and an inability to wake up)
- Frustration or irritability
Perception and sensation symptoms of TBI
- Light-headedness, dizziness, vertigo, or loss of balance or coordination
- Blurred vision
- Hearing problems, such as ringing in the ears
- Unexplained bad taste in the mouth
- Sensitivity to light or sound
- Mood changes or swings, agitation, combativeness, or other unusual behavior
- Feeling anxious or depressed
- Fatigue or drowsiness, including a lack of energy or motivation
TBI in children
Children might be unable to let their caregivers know that they feel different following a blow to the head. It’s important for adults to pay attention to a child’s behavior and ask about possible symptoms following a TBI. A child with a TBI may display the following signs or symptoms:
- Changes in eating or nursing habits
- Persistent crying, irritability, or crankiness—specifically with an inability to be consoled
- Changes in ability to pay attention
- Lack of interest in a favorite toy or activity
- Changes in sleep patterns
- Seizures
- Sadness
- Loss of a skill, such as toilet training
- Loss of balance or unsteady walking
- Vomiting
TBI’s effects on consciousness
A TBI can cause problems with consciousness, awareness, alertness, and responsiveness. Generally, there are four abnormal states that can result from a severe TBI:
- Minimally conscious state: People in this state still show some evidence of self-awareness or awareness of their environment (such as following simple commands and giving yes or no responses).
- Unresponsive wakefulness syndrome (UWS): This is a result of widespread damage to the brain. People with UWS are unconscious and unaware of their surroundings. But they can have periods of unresponsive alertness and may groan, move, or show reflex responses.
- Coma: A person in a coma is unconscious, unaware, and unable to respond to their environment, such as pain or light. A coma generally lasts a few days or weeks. After, the person may regain consciousness, die, or move into a vegetative state.
- Brain death: The lack of measurable brain function and activity after an extended period of time is called brain death. It can be confirmed by tests that show blood is not flowing to the brain.
How does TBI affect the brain?
TBI-related damage can stay in one area of the brain—known as a focal injury—or it can happen over a more widespread area—known as a diffuse injury. The type of injury also affects how the brain is damaged. The types of damage usually seen in the brain from a TBI include bleeding, swelling, and tearing that injures nerve fibers. This damage can cause inflammation, swelling, and metabolic changes.
Diffuse axonal injury (DAI)
DAI is one of the most common types of TBIs. It refers to widespread damage to the brain's white matter. DAI commonly happens in auto accidents, falls, or sports injuries.
DAI can disrupt and break down communication among nerve cells in the brain. It also leads to the release of brain chemicals that can cause further damage. Brain damage may be temporary or permanent and recovery can take a long time.
Concussion
A concussion is a type of mild TBI that may be considered a temporary injury to the brain but could take minutes to several months to heal. Causes of concussion may include a blow to the head or a rapid movement of the brain within the skull—which can happen when a person is violently shaken.
Someone with concussion either suddenly loses consciousness or their state of consciousness or awareness changes suddenly. A second concussion closely following the first one—the so-called “second hit” phenomenon—can lead to permanent damage or even death in some cases. Post-concussion syndrome involves symptoms that last for weeks or longer.
Hematomas
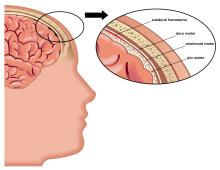
Hematomas are bleeding in and around the brain caused by a burst blood vessel. Different types of hematomas form depending on where the blood collects in the protective membranes surrounding the brain, which include the dura mater (outermost), arachnoid mater (middle), and pia mater (innermost). Specific types of hematomas include:
Epidural hematomas, which involve bleeding into the area between the skull and the dura mater. These can happen within minutes to hours after injury and are particularly dangerous.
Subdural hematomas, which involve bleeding between the dura and the arachnoid mater, and, like epidural hematomas, exert pressure on the outside of the brain. They are very common in older adults after a fall.
Subarachnoid hemorrhage, which is bleeding between the arachnoid mater and the pia mater.
Intracerebral hematoma, which involves bleeding into the brain itself and damages the surrounding tissue.
Contusions
Contusions are a bruising or swelling of the brain that happen when very small blood vessels bleed into brain tissue. Contusions can happen directly under the impact site (a coup injury) or, more often, on the complete opposite side of the brain from the impact (a contrecoup injury).
Contusions can appear after a delay of hours to a day. These generally happen when the head abruptly decelerates, which causes the brain to bounce back and forth within the skull (such as in a high-speed car crash or in shaken baby syndrome).
Skull fractures
Skull fractures are breaks or cracks in one or more of the bones that form the skull. They are a result of blunt force trauma and can cause damage to the membranes, blood vessels, and brain under the fracture. Helmets can help prevent skull fractures.
Chronic traumatic encephalopathy (CTE)
CTE is a progressive neurological disorder with symptoms that may include problems with thinking, understanding, and communicating. People may also experience movement disorders, problems with impulse control, depression, confusion, and irritability.
While CTE was originally identified only at autopsy, research to date suggests repeated TBIs may cause CTE. It develops over years and can take years to show symptoms.
Studies of retired boxers have shown that repeated blows to the head can cause issues including memory problems, tremors, lack of coordination, and dementia. Recent studies have demonstrated cases of CTE in other sports with repetitive mild head impacts (such as soccer, wrestling, football, and rugby). NINDS supports ongoing research to refine the diagnostic criteria for CTE.
Post-traumatic dementia (PTD)
PTD can happen after a single, severe TBI. PTD may be progressive and share some features with CTE. Studies assessing patterns among large populations of people with TBI show that moderate or severe TBI in early or mid-life may be associated with increased risk of dementia later in life.
Secondary damage
Initial damage to the brain can cause secondary damage. Secondary damage refers to the changes that happen over a period of hours to days after the primary injury. Examples of secondary damage include:
- Hemorrhagic progression of a contusion (HPC), which are injuries that happen when a contusion continues to bleed in and around the brain and expand over time. This creates a new or larger lesion and leads to swelling and further brain cell loss.
- A breakdown in the blood-brain barrier, which refers to the disruption of the network that controls the movement of cells and molecules between the blood and fluid that surrounds the brain's nerve cells. Once the blood-brain barrier is disrupted, blood, plasma proteins, and other foreign substances leak into the space between neurons in the brain. This triggers a chain reaction that causes brain swelling. It also causes inflammatory responses which can be harmful to the body if they continue for an extended period of time and the inappropriate release of neurotransmitters, which can damage or kill nerve cells.
- Increased intracranial pressure, which is usually caused by brain swelling inside the skull as a result of the injury. This pressure can damage brain tissue and prevent blood flow to the brain, depriving it of the oxygen it needs to function.
Other secondary damage can be caused by infections to the brain, low blood pressure or oxygen flow as a result of the injury, hydrocephalus, and seizures.
Who is more likely to get a traumatic brain injury?
Adults 65 and older are at greatest risk for being hospitalized and dying from a TBI, most often from a fall. In every age group, serious TBI rates are higher for men than for women. Men are more likely to be hospitalized and are nearly three times more likely to die from a TBI than women.
Anyone can experience a TBI. The leading causes of TBI include:
- Falls: According to the Centers for Disease Control and Prevention (CDC), falls are the most common cause of TBIs and happen most often among the youngest and oldest age groups.
- Blunt trauma accidents: Accidents that involve being struck by or against an object, particularly sports-related injuries, are a major cause of TBI.
- Vehicle-related injuries: Pedestrian-involved accidents, as well as accidents involving motor vehicles and bicycles, are the third most common cause of TBI.
- Assaults and violence: Abuse-related TBIs result from intimate partner violence, assaults, shaken baby syndrome, and wounds to the head caused by gunshots or other weapons.
- Explosions and blasts: TBIs caused by blast trauma from roadside bombs have become a common injury to service members in military conflicts. The majority of these TBIs are classified as mild head injuries.
How is a traumatic brain injury diagnosed and treated?
Preventing TBI
The best treatment for TBI is prevention. Unlike most neurological disorders, TBIs are preventable. The following actions can help prevent them:
- Wearing a seatbelt
- Wearing a helmet when riding a bicycle, skateboarding, and playing sports like hockey and football. Make sure it is the appropriate helmet for the activity and that it fits correctly.
- Never driving under the influence of drugs or alcohol
- Improving balance and strength with a regular physical activity program
There also changes in the home that can prevent falls, such as:
- Installing window guards and safety gates for young children
- Improving lighting and removing rugs, clutter, and other trip hazards in hallways
- Using nonslip mats and installing grab bars next to toilets and in tubs or showers, especially for older adults
- Installing handrails on stairways
Diagnosing TBI
All TBIs should be evaluated immediately by a professional who has experience with these injuries. A neurological exam will judge motor and sensory skills and test hearing and speech, coordination and balance, mental status, and changes in mood or behavior, among other abilities.
Screening tools developed for coaches and athletic trainers can identify the most concerning concussions for medical evaluation.
Medical providers can use brain imaging to evaluate the extent of primary TBIs and determine if a person will need surgery to help repair any damage to the brain. A physical examination by a doctor and the person's symptoms will help determine whether imaging is needed. Commonly used imaging for TBI includes CT (computed tomography) and MRI (magnetic resonance imaging). CT imaging can show a skull fracture and any brain bruising, bleeding, or swelling. MRI is more sensitive and can pick up more subtle brain changes that a CT scan may miss.
Learn more about neurological diagnostic tests and procedures.
Significant advances in neuroscience research and imaging technology over the last decade have developed non-invasive methods (don’t enter the body) with higher resolution to detect milder TBI damage. Researchers may use:
- Diffusion tensor imaging, which could identify damage in white matter tracts in the brain
- Fluid-attenuated inversion recovery, which could detect small areas of damage
- Susceptibility-weighted imaging, which could identify even small and hard to detect brain bleeds
Even though there are advances in imaging resolution, currently available and clinically validated imaging technologies, blood tests, and other measures can’t always detect damage from mild, concussive injuries.
Neuropsychological tests to gauge brain functioning are often used along with imaging in people who have suffered mild TBI. Such tests involve performing specific tasks that help assess memory, concentration, information processing, executive functioning, reaction time, and problem solving.
Many athletic organizations recommend establishing a baseline picture of an athlete's brain function at the beginning of each season, ideally before any TBIs happen. Brain function tests provide information about a person’s memory, attention, and ability to concentrate and solve problems.
Brain function tests can be repeated at regular intervals (every one to two years) and also after a suspected concussion. The results may help healthcare providers identify any effects from an injury and allow them to make more informed decisions about whether a person is ready to return to their normal activities.
Treating TBI
Many factors—including the size, severity, and location of the injury—influence how TBI is treated and how quickly a person might recover. Although brain injury often happens at the moment of head impact, much of the damage related to severe TBI develops from secondary injuries which happen days or weeks after the initial trauma. For this reason, people who receive immediate medical attention at a certified trauma center tend to have the best health outcomes.
Genetics may play a role in how quickly and completely a person recovers from a TBI. For example, researchers have found that apolipoprotein E ε4 (APOE4)—a genetic variant associated with higher risks for Alzheimer's disease—is associated with worse health outcomes following a TBI. Much work remains to be done to understand how genetic factors—as well as specific types of TBIs—affect recovery.
Studies suggest that age and the number of TBIs a person has suffered over his or her lifetime are two critical factors that impact recovery. Brain swelling in newborns, young infants, and teenagers often happens much more quickly than it does in older people. Evidence from very limited CTE studies suggest that younger people (ages 20 to 40) tend to have more behavioral and mood changes with CTE, while those who are older (ages 50+) tend to have more cognitive difficulties.
Compared with younger adults with the same TBI severity, older adults are more likely to have lasting symptoms. Older people often have other medical issues and may be taking multiple medications, which may complicate treatment. For example, blood thinning medications may increase the risk of bleeding in the brain.
Mild TBI
Some people with mild TBI (such as a concussion) may not require treatment other than rest and over-the-counter pain relievers. Treatment should focus on symptom relief and “brain rest.” Brain rest means avoiding activities that require concentration or attention. The person should be monitored by their healthcare provider to note new or worsening symptoms.
Children and teens who have a sports-related concussion should stop playing immediately and return to play only after being approved by a concussion specialist.
Preventing future concussions is critical. While most people recover fully from a first concussion within a few weeks, the rate of recovery from a second or third concussion is generally slower.
Even after concussion symptoms go away, people should return to their daily activities gradually, and only once they have permission from a doctor. While there are some guidelines available, further research is needed to better understand the effects of mild TBI on the brain and determine when it’s safe to resume normal activities.
People with mild TBI should:
- Make an appointment for a follow-up visit with their healthcare provider to confirm the progress of their recovery.
- Talk about new or ongoing symptoms and ask how to treat them.
- Pay attention to any new signs or symptoms even if they seem unrelated to the injury (for example, mood swings or unusual feelings of irritability). These symptoms may be related even if they happen several weeks after the injury.
Medications to treat symptoms of TBI may include:
- Over-the-counter or prescribed pain medicines
- Anticonvulsant drugs to treat seizures
- Anticoagulants to prevent blood clots
- Diuretics to help reduce fluid buildup and reduce pressure in the brain
- Stimulants to increase alertness
- Antidepressants and anti-anxiety medications to treat depression and feelings of fear and nervousness
Severe TBI
Immediate treatment for someone who has a severe TBI focuses on:
- Preventing death
- Stabilizing the person's spinal cord, heart, lung, and other vital organ functions
- Ensuring proper oxygen delivery and breathing
- Controlling blood pressure
- Preventing further brain damage
Emergency care staff will monitor the flow of blood to the brain, brain temperature, pressure inside the skull, and the brain's oxygen supply.
A person with severe TBI may need surgery to:
- Relieve pressure inside the skull
- Remove debris, dead brain tissue, or hematomas
- Repair skull fractures
Rehabilitation for severe TBI
Once their injuries are treated and stabilized in the hospital, people with severe TBI are often transferred to a rehabilitation center where a multidisciplinary team of providers help with recovery. The rehabilitation team may include:
- Neurologists
- Nurses
- Psychologists
- Nutritionists
- Physical therapists
- Occupational therapists
- Vocational therapists
- Speech therapists
- Respiratory therapists
Therapy is aimed at improving the person's ability to perform activities of daily living and to address cognitive, physical, occupational, and emotional difficulties. Treatment may be needed on a short- or long-term basis.
What are the latest updates on traumatic brain injury?
NINDS, a part of the National Institutes of Health (NIH), is the leading federal funder of research on the brain and the nervous system, including disorders such as TBI. NINDS, along with other NIH institutes, supports new and innovative research to better understand, diagnose, and treat TBI.
NINDS-funded research includes studies to understand TBI and its associated conditions, studies to improve diagnosis and outcomes, and studies to develop potential therapies for TBI. Projects are currently:
- Exploring ways to promote the brain's natural ability to adapt and repair itself, known as neuroplasticity
- Refining diagnostic criteria for both CTE and the associated Traumatic Encephalopathy Syndrome (TES)
- Supporting the development and validation of clinically relevant biomarkers (biological signs of disease that can be found and measured) for TBI through the Translational Outcomes Project in Neurotrauma (TOP-NT) consortium
- Identifying biomarkers for CTE in order to detect this and similar disorders in living people rather than through autopsy after death
Clinical research
NINDS co-leads the Strategies to Innovate EmeRgENcy Care Clinical Trials (SIREN) network. This network supports projects that include TBI trials—one of which is BOOST3 (Brain Oxygen Optimization in Severe TBI). Through BOOST3, scientists are comparing two methods for monitoring brain tissue oxygen to determine the best treatment approach for people with TBI.
The recently completed NINDS-funded Transforming Research and Clinical Knowledge in TBI, or TRACK TBI, project was an observational study of adults and children with TBI at all levels of injury severity. It provided a TBI database as well as tools and resources to establish more precise methods to diagnose it and improve ways to assess a person’s outcomes after an injury. Now, researchers are extending the study by continuing to follow study participants in an effort to identify risk factors and biomarkers for TBI and to learn more about outcomes for people with TBI.
Harnessing the efforts of the many physicians and scientists working on developing better treatments for TBI requires that everyone collect the same types of data, including details about injuries and treatment results. NINDS's Common Data Elements project brings the research community together to develop data collection standards.
Scientific collaboration in TBI research
NINDS and the European Commission conduct studies through the International Initiative for TBI research (InTBIR), which seeks to improve diagnosis and evaluate which types of care are associated with the best outcomes in children and adults.
NIH and the Department of Defense together lead the Federal Interagency TBI Research (FITBIR) database, which includes data from observational and other studies.
NIH investigators and the FDA are active collaborators in the Department of Defense-led TBI Endpoints Development (TED) program to develop better designed clinical trials to lead to effective treatments for TBI.
NINDS also works with the Department of Defense and the Departments of Health and Human Services, Veterans Affairs, and Education to coordinate TBI research for military members. The associated National Research Action Plan (NRAP) aims to improve prevention, diagnosis, and treatment of TBI and other conditions (such as PTSD) that affect veterans and their families.
To advance research on TBI, it’s important that classification of the types of TBI is precise and evidence-based. This would go beyond the currently used "mild," "moderate," and "severe," designations. In January 2024, NINDS held the TBI Classification and Nomenclature Workshop to support these efforts.
For more information on research about TBI, check NIH RePORTER, a searchable database of current and past research projects supported by NIH and other federal agencies. RePORTER also has links to publications and resources from these projects.
For research articles and summaries on TBI, search PubMed, which contains citations from medical journals and other sites.
How can I or my loved one help improve care for people with traumatic brain injury?
Consider participating in a clinical trial so clinicians and scientists can learn more about TBI and related disorders. Clinical research with human study participants helps researchers learn more about a disorder and perhaps find better ways to safely detect, treat, or prevent disease.
All types of participants are needed—those who are healthy or may have an illness or disease—of all different ages, sexes, races, and ethnicities. This helps make sure that study results apply to as many people as possible, and that treatments will be safe and effective for everyone who will use them.
For information about participating in clinical research visit the NINDS Clinical Trials site and NIH Clinical Research Trials and You. Learn about clinical trials currently looking for people with TBI at ClinicalTrials.gov, a searchable database of current and past clinical studies and research results.
People with a TBI can also support research by designating the donation of brain tissue before they die. Human brain tissue is essential to increasing the understanding of how the nervous system functions. The NIH NeuroBioBank is an effort to coordinate the network of brain banks it supports across the country to advance research through the collection and distribution of post-mortem brain tissue to qualified research teams.
Where can I find more information about traumatic brain injury?
Information may be available from the following sources:
