The link between high blood pressure and dementia
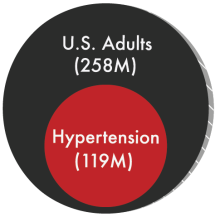
Emerging research underscores the connection between uncontrolled high blood pressure, stroke, and an increased risk of dementia. Managing blood pressure effectively can help lower the risk of dementia and maintain brain health.
What the science says:
- Early intervention is key: Managing blood pressure as early as your late 20s can prevent damage to brain blood vessels.
- Consistent care yields better outcomes: Long-term blood pressure control is linked to a lower risk of cognitive decline, memory problems, and dementia.
- Treatment shows cognitive benefits: Studies such as SPRINT MIND show that intensive blood pressure treatment can reduce the risk of mild cognitive impairment. [ref.] [ref.]
The impact of blood pressure control
Improving blood pressure control across populations could dramatically reduce the number of dementia cases. Even preventing a small percentage of cases has significant public health and economic benefits, not to mention the benefits to individuals and their loved ones.
Promoting healthy brain aging
High blood pressure is a major risk factor for brain blood vessel disease. Controlling it can help prevent strokes and reduce the risk of cognitive decline. Research suggests that managing blood pressure in midlife is particularly effective in preserving brain health and function.
Ongoing research needs: Numerous studies are investigating the relationship between vascular disease and cognitive function. These include antihypertensive medications, lifestyle interventions, and biological mechanisms linking high blood pressure to dementia. But to reduce dementia rates, public health efforts must increase education and awareness among those most at risk. [ref.] [ref.] [ref.] [ref.] [ref.]
Potential health and financial benefits of blood pressure control
Controlling high blood pressure is a cost-effective, evidence-based strategy with wide-reaching benefits for both population health and healthcare systems. Addressing hypertension in midlife can help delay or prevent stroke and dementia, two leading contributors to disability, long-term care needs, and healthcare spending. Investing in prevention through early detection, equitable treatment access, and lifestyle support yields dividends not only in longer, healthier lives but also in reduced economic burden across sectors.
Improved blood pressure control supports healthy brain aging
Extensive research shows that effective blood pressure management can reduce the incidence of stroke, slow the progression of white matter disease, and lower the risk of developing both vascular dementia and Alzheimer’s disease. Early and sustained intervention—particularly between the ages of 28 and 45—helps preserve cognitive function into older age. Population-level efforts to improve hypertension awareness and treatment adherence are critical to promoting healthy brain aging and reducing age-related cognitive decline.
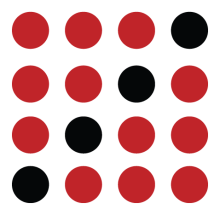
Over the past five decades, stroke rates in the U.S. have declined by more than 70%—a trend strongly linked to improved hypertension control as a standard of care (CDC). If vascular disease contributes to dementia risk, as evidence suggests, then improvements in stroke prevention should also reduce dementia incidence. Multiple studies have found that dementia rates have decreased by roughly 13% per decade in high-income countries, including the United States (Harvard T.H. Chan School of Public Health).
Preventing cognitive decline reduces long-term care and economic burden
The worldwide cost of dementia was estimated at $818 billion in 2015—a figure projected to rise sharply as the population ages (Population Reference Bureau). Meanwhile:
Compounding the problem, public awareness of hypertension has declined in recent years, from 85% in 2013–2014 to just 77% in 2017–2018 (NIH).
Improving blood pressure control across the population is one of the most promising evidence-based ways to reduce the risk of dementia, alleviate pressure on long-term care systems, and contain public and private healthcare spending.
Key headlines and references on blood pressure and cognitive decline
*JAMA - Journal of the American Medical Association
JAMA:Blood pressure control in the U.S. is slipping and raising long-term dementia risk
After years of progress, blood pressure control among U.S. adults with hypertension declined between 2013 and 2018. This trend is concerning because poor hypertension control increases lifetime risk for stroke and dementia.
JAMA: Intensive blood pressure treatment may help delay the early signs of dementia
The SPRINT MIND randomized trial found that lowering blood pressure more aggressively significantly reduced the incidence of mild cognitive impairment, a common early indicator of dementia, reinforcing the importance of midlife intervention.
JAMA: Lower blood pressure slows damage to the brain's white matter
This follow-up to the SPRINT MIND trial used brain imaging to show that intensive blood pressure control reduced progression of white matter lesions—areas of structural brain damage linked to cognitive decline and vascular dementia.
National Academies of Sciences: Midlife blood pressure control is a promising tool for dementia prevention
A consensus report by the National Academies concluded that managing blood pressure during midlife could help prevent or delay cognitive decline. While evidence is not definitive, the benefit-to-risk ratio supports making it a public health priority.
The Lancet: As much as 40% of dementia cases may be preventable
The Lancet Commission identified high blood pressure as one of 12 modifiable risk factors and emphasized that early interventions—especially in midlife—could significantly reduce global dementia incidence.
The Lancet: Blood pressure medications reduce dementia risk, regardless of drug type
This large meta-analysis of individual-level data found that antihypertensive medications significantly reduce the risk of both dementia and Alzheimer’s disease. The benefit is held across different medication classes, supporting treatment flexibility.
Hypertension: Black Americans experience faster cognitive decline with high blood pressure
In this 8-year longitudinal study, higher systolic blood pressure was associated with greater cognitive decline, particularly among Black participants. The findings underscore racial disparities and the urgency of targeted prevention.
JAMA: Midlife vascular risk factors predict dementia 25 years later
This long-term cohort study from the ARIC project found strong associations between midlife hypertension and late-life dementia. It reinforces the importance of prevention decades before symptoms appear.