
Naomi Lee, Ph.D.
Seneca Nation
NIH IRACDA-ASERT Postdoctoral Fellow
Department of Molecular Genetics and Microbiology
University of New Mexico
UNM Biomedical Research Education Programs ASERT-IRACDA Fellows
Building my identity as a Native American scientist
When I started studying science in college, I didn’t consider myself a “Native woman in STEM.” I didn’t think I was smart enough, or good enough, or even Native enough, since I am only half. As I got older, even once I began considering myself a Native woman, I thought of my identities as separate: I was a Native woman and I was a scientist. My postdoc at the NIH and the mentorship I received there helped me unite these identities; I finally consider myself a Native female scientist. To me, that means having the cultural knowledge and scientific training to help my people. Once I understood who I am and what I am capable of doing, my career trajectory completely changed—for the better.
I was raised on the Seneca Cattaraugus Indian reservation located south of Buffalo, NY. I had little exposure to career opportunities on the reservation and the small rural towns that surrounded it. However, I became interested in science at an early age because my parents had myself and my siblings participate in after school and summer activities through the local high school.
I attended Rochester Institute of Technology (RIT) and majored in biochemistry. At the time, I didn’t even know what graduate school was; as a first-generation college student, my parents were just thrilled for me to finish college. Dr. Jason Younker, an anthropologist and the first Native American Ph.D. that I have met was hired at RIT. He immediately stepped up and became my first mentor and encouraged me to participate in the American Indian Science and Engineering Society (AISES) conferences along with participating in research at RIT. From these experiences, I became excited about a career as a scientist.
After college, I joined the Ph.D. program in chemistry at the University of Rochester. Once I finished my Master’s degree, I took a leave of absence to care for my parents. During those two years, I joined the Army National Guard and went to Officer Candidate School at Fort Benning, GA. The Army continues to benefit me as a scientist, providing me with leadership and organizational skills and the ability to work under pressure. Once you’ve been responsible for the lives of 100 soldiers, performing cell culture is low-stakes. The time away from the lab also made me realize how much I enjoyed science; I missed the variety and intellectual stimulation. When I returned to graduate school, it was with a new appreciation for the work.
My Ph.D. focused on proteins and peptide self-assembly, but I wanted my postdoc to focus on in infectious diseases and the role that proteins play in disease. I connected with Dr. Clif Poodry, a Native American scientist who was at NIGMS at the time, and through his networks I was recommended to Dr. Steven Jacobson, senior investigator in the NINDS intramural program.
My postdoctoral research in Dr. Jacobson’s lab focused on treatment and detection of human herpesvirus-6. At NINDS, I had access to many renowned scientists along with excellent mentors, who helped me explore my interests and values and more purposefully shape my career. I also was exposed to state of the art technology and new lab techniques such as digital droplet PCR. The NIH intramural program is a great place to build your scientific and research skills.
I also learned the importance of matching your research question to the strengths of the institution you are in. While in my postdoc, I learned that there were viruses endemic to tribal communities that were not seen in other communities. This topic perfectly intersected with my interest in infectious disease and my desire to serve my community. However, the intramural program did not have the necessary research collaborations with tribal communities, so the project never got off the ground. Nevertheless, I was able to take advantage of other opportunities while I was at NIH to prepare me for that research in the future. For example, I completed an Institutional Review Board (IRB) internship in the Bioethics Department of the NIH Clinical Center that has been invaluable in my current work with tribal communities.
I am now participating in the NIH Institutional Research and Academic Career Development Award (IRACDA) program at the University of New Mexico. I am a postdoctoral fellow in the lab of Dr. Bryce Chackerian, doing research on the identification and development of potential Neisseria gonorrhoeae vaccine candidates using virus-like particles to display peptide libraries. I am also part of the NIH-funded Native Investigator Development Program, through which I am researching human papillomavirus prevalence and risk factors within the American Indian women of the Northern Plains.
My long-term career goal is to pursue an independent research career that will focus on novel vaccine development. I also want to improve the healthcare of the Native American community through community-based participatory research, STEM education, and outreach. I developed that clarity of purpose through the guidance of mentors, and my advice is: don’t be afraid to ask for help or make mistakes. No one can get far in their career alone and often the best discoveries come from mistakes.
Current Research
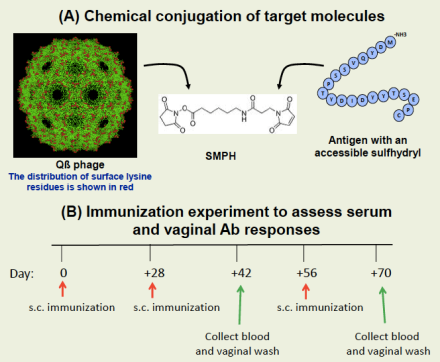
A successful gonorrhea vaccine must target conserved antigens and elicit protective mucosal immune responses. We have identified five promising vaccine candidates in the form of synthetic peptides that elicit antibodies that recognize a diverse collection of gonorrhea strains, bind to the surface of the virus, and are bactericidal against highly serum-resistant strains. However, progress has been stymied by the inability of these peptides to induce a vaginal antibody response when given by injection or nasally.
We are now experimenting with an antigen delivery system, called virus-like particles (VLPs), that allows for repetitive display of peptide antigens with the goal of eliciting high-titer vaginal antibody response at low doses. Our research with VLPs displaying an HPV peptide was able to protect mice from experimental genital HPV infection, and we hope to employ similar tactics for gonorrhea.
