Edjah K. Nduom, MD
Assistant Clinical Investigator
Surgical Neurology Branch
National Institute of Neurological Disorders and Stroke
National Institutes of Health
From bench to bedside and back: Balancing a career in medicine and science
I have always been interested in how things work. I was the kid who was thrilled to get a science kit when I was growing up, because of all of the fun experiments that you could run. From the time I was little, I knew I wanted to do something challenging as a career, something that presented a new problem to solve on a daily basis. After I started telling friends and relatives that I would become a brain surgeon, one of my aunts gave me the book “Gifted Hands,” the autobiography of neurosurgeon Ben Carson, and that cemented my youthful ambition.
During college, I was interested in science, but I did not really have any interest in being a scientist, per se. I liked the idea of using my hands to solve difficult problems for people as a neurosurgeon, but the science seemed too risky – what if you never discover anything? Would you have wasted your time? Then, before my sophomore year, I went to a three week seminar with a developmental neurobiologist at Stanford, Susan K. McConnell, PhD. Over the course of the seminar, she took us through seminal discoveries in neuroscience and asked us to imagine how we would have solved the same problems. How we could figure out, for example, how nerves managed to send projections from the eye to the vision center of the brain? She guided us through coming up with a set of hypothetical experiments, and then showed us how these things had actually been discovered. It was a tremendously stimulating experience, and when it ended, I asked her if I could work in her lab. I worked with her through my next two years at Stanford and was awarded a grant to work in her lab over the summer break after sophomore year.
After that experience, I realized there was so much that we did not yet know about the brain, and I wanted to help figure it out. From then on, I prioritized getting research experience during my medical training. One such experience came about by happenstance; during residency, while at a neurosurgery conference, I heard Russell Lonser, MD, who was then the Chief of the Surgical Neurology Branch at NINDS, explain how neurosurgeons at the NIH were using catheters implanted directly into the brain to bypass the blood-brain barrier. As a budding neurosurgeon, I was hooked; I knew that surgery, while a critical part of treatment, would never be enough on its own to cure malignant tumors. This technique provided another way for surgeons to directly affect the treatment of brain tumors and complement the work of oncologists and radiologists.
I applied for and was awarded an eight month Clinical Fellowship at the NIH to work with Dr. Lonser. While at the NIH, I was exposed to grant-writing workshops and scientific writing workshops – these courses and the process of writing and publishing my first two first author original science articles helped me realize that spreading science to others required more than data – you needed to tell a convincing story, show the reader how you went from an idea to an answer. That experience was also when I knew that I could start and complete a project that I conceived of myself.
After my residency, I spent two years at UT MD Anderson Cancer Center before returning to the NIH as a Staff Clinician. I am currently a neurosurgical oncologist in the Surgical Neurology Branch of the National Institute of Neurological Disorders and Stroke. I operate on patients with brain tumors, and then I study their tumors for weaknesses, so that we can find better ways to treat these tumors in the future.
I chose to start my career at the NIH because it is one of the few places in the country with the resources to support a neurosurgeon-scientist. Neurosurgery is one of the most time-consuming specialties in medicine—as a surgeon, a large part of my time will always be taken up with patient care. At NIH, I am not under pressure to do surgeries to bring in revenue— they want me to do as much clinical activity as will drive my science and help patients, to do what I need to do to make a difference in brain tumors. That means I can spend more time thinking about my science and working with my research staff.
To run a lab on top of being a practicing physician can be a challenge, but it comes with advantages both scientific and personal. Being the one to see the patient and surgically resect the tissue that will be used in my experiments means I have a much more complete understanding of how our findings in the lab relate to the bigger picture of a patient’s overall care. Personally, I also get a balance of the long-term, creative work of doing cutting-edge science and the instant gratification of completing a surgery and directly helping a patient.
I would encourage anyone interested in science to seek out people who are doing the work that fascinates them, people who are truly pushing the envelope in the field. Don’t be afraid to stop someone after a talk or a lecture, even if you think you don’t have a great question. In my life, such random encounters have led to several productive and ongoing mentoring relationships.
Current Research
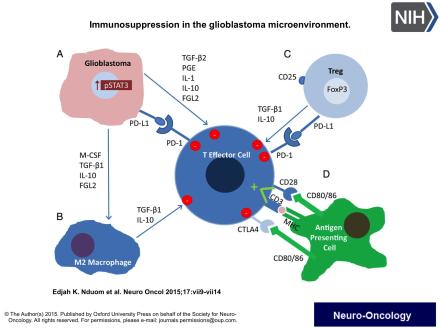
My work centers on trying to harness the power of the immune system to fight brain tumors. Our immune system is the body’s primary way of fighting off infections, but it is also constantly active monitoring the cells of our bodies for abnormalities. In this way, the immune system is also the front line of defense against the abnormal cells of cancer. Unfortunately, many cancers have found ways to hide themselves from the immune system. In the attached figure, you can see the many ways that brain tumors send signals that shut down the effector T cells that the immune system sends to fight tumors. By studying the many ways that tumors do this in real patients, I help discover ways that we can evade these defenses and use the body’s own defenses to ward off cancer.
