
Azizi Seixas, Ph.D.
Assistant Professor of Population Health Center
for Healthful Behavior Change
NYU Langone Health
Addressing inequality through multidisciplinary training and research
The seed of my scientific journey was planted as a child growing up in inner-city Jamaica, when I became acutely aware of how different the worlds of the “haves” and the “have nots” were. I knew this inequality well because I was one of the “have nots,” growing up in a single-parent home in one of the poorest neighborhoods in Jamaica, while attending one of the most affluent high schools on an academic scholarship. When I emigrated to the U.S. to pursue a career in science, I realized that a similar chasm existed between the “haves” and the “have nots” here in the U.S. The health of the “have nots”—often racial/ethnic minorities and low income populations, is far worse than individuals of the white or higher income groups. I felt that I could somehow make a difference in the lives of the “have nots” by improving their financial, psychological, and physical health. My research career has been a search for answers to these inequalities, using and ultimately integrating a variety of disciplines from philosophy to psychology to machine learning to tackle complex health questions in novel ways.
Like many undergraduates, I was initially drawn to a career in medicine. As I got more immersed in philosophy and psychology, my interests began to shift toward those subjects and I ultimately majored in philosophy with a premedical concentration. For my senior thesis capstone project, I lived with an indigenous community in Jamaica called the Maroons, performing ethnographic research on Junkanoo, a cultural practice celebrated across the world with African, European, and Native American roots. My current interest in community-based research, which takes a participatory approach by enlisting key stakeholders for input on the design of the research, stems from this experience.
After undergrad, I got my Master of Psychology from the University of Dallas. This degree focused more on the qualitative side of psychology, with a philosophy bent. When pondering my next step, I knew that the questions I was interested in would require an approach that integrated qualitative and quantitative research, the latter of which I had little experience in. Therefore, I went on to get my Master’s and PhD in clinical psychology from Fordham, which had an eclectic program that would provide an immersive research experience and build my quantitative and statistical skills. My internship year research was a psychiatric epidemiology study with Dr. Bruce Link at Columbia University, investigating the influence of community stressors and trauma on the onset and trajectory of psychiatric outcomes.
Subsequently, I had the choice of a teaching job and a postdoc at Columbia. Although committed to research, I chose to teach at Hostos Community College because my wife was pregnant, and the teaching salary was significantly higher. Still, I wanted to further develop my research skills. By serendipity, I found out about the NHLBI-funded Program to Increase Diversity among Individual Engaged in Health-Related Research (PRIDE) training program at NYU Langone Health. This program provides intensive mentored research training to junior faculty in behavioral medicine and sleep disorders research. I had just gotten my permanent resident status a few months earlier, and, fittingly, this program was one of the first things I applied to as a US resident. I wasn’t sure I would qualify because I was from a community college, not a research-intensive school, but I had to try. Happily, I was accepted.
That was a summer of full immersion. At first, I felt like an impostor. All the other participants were assistant professors at big name schools, while I had no idea what an R or K grant was. I was upfront about my ignorance, and the group was incredibly supportive and willing to work with me.
After that summer, the researchers I worked with, Drs. Girardin Jean-Louis and Gbenga Ogdegbe, found some synergy between our research interests. The NINDS-funded Center for Stroke Disparities Solutions was conducting a comparative effectiveness trial to reduce secondary stroke among racial/ethnic minorities, and I was interested in developing a research program focusing on sleep, brain health, and aging. We applied for and were awarded a diversity supplement from NINDS to fund my postdoctoral research, which added neuropsychological assessment of these stroke survivors to investigate the impact of neurocognitive and psychosocial impairments and sleep disturbance on stroke disability. Before I received the supplement, I was teaching 5 or 6 courses on top of conducting research; NINDS funding allowed me to devote all my time to becoming an independent scientist.
The supplement opened up so many training opportunities for me. I was especially interested in doing machine learning but didn’t have the resources at a community college to do that kind of work. My current work in the areas of machine learning, complex system science simulation modeling, and health-related “internet of things” solutions to tackle vexing health disparities issues can be directly attributed to my supplement funding. I became a better scientist and I am moving toward becoming an independent scientist. I learned critical grant-writing skills through mock grant reviews, which taught me how reviewers think and let me anticipate the criticisms I might encounter. Most importantly, I was able to submit a successful NHLBI K01 Mentored Career Award within a year and a half of the supplement and secure a faculty position at NYU. Although my journey has been circuitous, each of my experiences have shaped me as scientist and improved my scientific thinking.
- As told to Lauren Ullrich
Current Research
My research broadly focuses on three areas: 1) causes of sleep and cardiovascular disease (CVD) disparities, 2) long-term health consequences of cardiovascular disease disparities, and 3) developing adaptive, personalized behavior modification interventions to improve health and well-being. In particular, my research investigates whether insufficient sleep and/or obesity, which are two to three times more prevalent among blacks compared to whites, might explain a significant proportion of cardiovascular disease (CVD) risk disparity between blacks and whites. I am using machine learning to determine profiles of sleep and body-mass index that can be associated with lower CVD risk. Once these profiles are established, precision medicine approaches can be employed to create hypothetical treatments and find the most optimal treatment for a given individual.
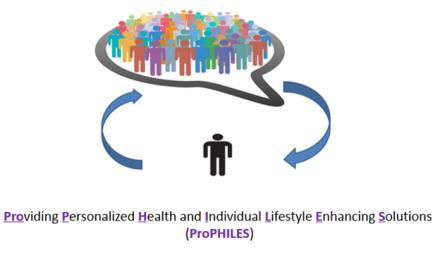
Providing Personalized Health and Individual Lifestyle Enhancing Solutions (ProPHILES) model.
